“Unraveling the complexities of private medical aid in South Africa is crucial for making informed healthcare decisions. This guide aims to demystify your scheme’s exclusions and limitations, empowering you to navigate the best private medical aid options available. Understanding these nuances ensures you’re prepared for unexpected medical expenses. We’ll explore common gaps in coverage, treatment restrictions, and how to maximize benefits, helping you choose a scheme that aligns with your unique health needs.”
Understanding Private Medical Aid Schemes in South Africa
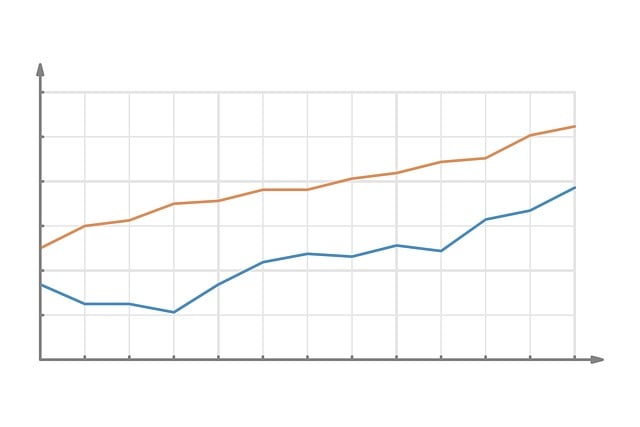
In South Africa, Private Medical Aid (PMA) schemes play a significant role in ensuring access to quality healthcare for individuals and families who opt for private medical cover. These schemes, offered by various insurance companies, are designed to cater to diverse healthcare needs, with options ranging from comprehensive to more niche packages. When considering the best private medical aid in South Africa, understanding your specific healthcare requirements is key. Each scheme has its unique set of benefits, exclusions, and limitations, making it crucial to read and comprehend the policy documents carefully.
The PMA schemes in South Africa typically cover a wide range of medical services, including outpatient consultations, hospital stays, specialist treatments, and prescription medications. However, not all plans offer the same level of coverage. Some schemes may exclude certain procedures or conditions, such as pre-existing illnesses, dental care, or alternative medicine practices. It’s essential to know these exclusions beforehand to avoid unexpected costs or limitations when seeking medical treatment.
– Overview of private medical aid and its significance in SA
Private medical aid, often considered the best option for comprehensive healthcare coverage in South Africa, plays a pivotal role in ensuring access to quality medical services. Given the country’s diverse landscape and population, this form of health insurance has become indispensable, offering individuals and families peace of mind and financial protection against unexpected medical expenses. In a nation with both vibrant urban centres and remote rural areas, the best private medical aid schemes cater to a wide range of healthcare needs, from specialist treatments in top-tier hospitals to preventive care in community clinics.
South Africa’s dynamic economy and robust healthcare sector drive the evolution of private medical aid plans, which are tailored to suit various demographics and lifestyles. These plans not only cover inpatient and outpatient care but also extend to vital services such as maternity, dental, and mental health support, ensuring that members have access to a full spectrum of healthcare solutions. Understanding the specific exclusions and limitations within these schemes is crucial for subscribers to make informed decisions regarding their health and wellness.
– Types of schemes available and how they differ
In South Africa, private medical aid schemes offer a range of options for individuals seeking comprehensive healthcare coverage. The best private medical aid in South Africa typically falls into two main categories: open and closed schemes. Open schemes are known for their flexibility, allowing members to choose any healthcare provider within the scheme’s network, including public hospitals and private clinics. This option provides wide access to medical services and is often preferred by those who value freedom of choice. Conversely, closed schemes have a more restricted network of healthcare providers, usually consisting of a specific set of private hospitals and specialists. While this may limit choices, closed schemes often offer lower co-payments and faster access to treatment due to the pre-approved nature of the provider network.
When considering the best private medical aid in South Africa, it’s crucial to understand that each scheme has its own set of inclusions and exclusions. Inclusions refer to the medical services covered under the scheme, while exclusions are treatments or procedures not provided. Some schemes may exclude specific conditions like pre-existing illnesses, while others might not cover certain specialty services. Members should carefully review their scheme’s terms and conditions to ensure it aligns with their healthcare needs and preferences.